Bowing out of the Tournament
Author: Evon Looper, MD, PGY1; Ramesh Karra, MD
Peer-Reviewer and Final Editor: Will Denq, MD, CAQ-SM
A 15-year old male presents with right elbow pain and deformity after injury sustained during a wrestling tournament. He has a large joint effusion and prominent olecranon, and is otherwise neurovascularly intact.


Image 1. Plain radiographs of the right elbow taken on initial presentation after unsuccessful conscious reduction attempt in the field. Author’s own images.
What is the diagnosis?
Acute traumatic posterolateral elbow dislocation.
What is the mechanism of injury?
Elbow dislocations typically occur as a result of a fall onto an outstretched arm with the elbow extended. This mechanism most commonly results in a posterolateral dislocation pattern [3]. In a wrestling match, this injury may occur when an athlete is thrown and reflexively extends their arm to cushion or redirect their fall.
Which fracture is most commonly associated with this injury in the pediatric population?
The most common fracture associated with this injury is an avulsion of the medial humeral epicondyle, which occurs in approximately 30-60% of cases [3]. The medial epicondyle is the last ossification center to fuse in the distal humerus, making it vulnerable to avulsion when the ulnar collateral ligament experiences high tension during dislocation [2].
-
Pearl: It may be difficult to differentiate between fractures and normal ossification centers when interpreting plain films in the pediatric population. To aid with this, “CRITOE” is a useful mnemonic for the appearance of ossification centers within the elbow, with letter positioning corresponding to age of appearance. The simplified counting method is with average ages of 1-3-5-7-9-11, which correspond to the capitellum (C) appearing at age 1, radial head (R) at age 3, internal epicondyle (I) at age 5, trochlea (T) at age 7, olecranon (O) at age 9, and external epicondyle (E) at age 11 [6].

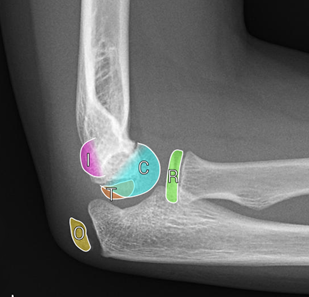
Image 2. Elbow ossification centers: capitellum (C), radial head (R), internal (medial) epicondyle (I), trochlea (T), olecranon (O), and external (lateral) epicondyle (E). Case courtesy of Leonardo Lustosa, Radiopaedia.org, rID: 80555.
What is a dangerous complication of this fracture?
Incarceration of the fracture fragment within the elbow joint. This may be a result of the initial dislocation, occurring after spontaneous joint reduction, or be the sequelae of a reduction attempt. If left untreated, long-term complications such as chronic pain, limited range of motion, joint instability, and ulnar nerve injuries may develop. Therefore, it is imperative to obtain pre- and post-reduction plain films to evaluate for incarcerated fragments [5].


Image 3. Plain radiographs of the right elbow taken after closed reduction attempt. Medial epicondyle fracture fragment visualized within the ulnohumeral joint space. Author’s own images.
-
Pearl: The presence of a fracture fragment within the elbow joint is an absolute indication for urgent operative repair and, therefore, orthopedic surgery should be consulted if identified. These may be difficult to identify on plain film and a general rule is that any medial epicondyle fragment appearing at the level of the joint should be considered incarcerated until proven otherwise. Additionally, failed reduction, incomplete reduction, or reduction followed by a decrease in elbow extension or ulnar nerve palsy may indicate an incarcerated fragment [2].
What is the recommended management in the ED?
Simple posterolateral elbow dislocations are treated with closed reduction in the emergency department, often under procedural sedation, followed by immobilization in a long arm splint until orthopedic follow-up within two weeks to prevent elbow stiffness [4]. Here’s a short video that describes elbow hematoma block administration and a technique of closed reduction of a simple posterolateral elbow dislocation. For complex dislocations, orthopedic consultation is warranted and operative intervention may be required. Common reduction techniques include a combination of elbow hyperextension, longitudinal traction, forearm supination, and elbow flexion [3]. Reduction in this patient was achieved by holding the forearm in supination while applying longitudinal traction with counter-traction, medial pressure on the radial head, and gentle elbow flexion.
-
Pearl: Incarcerated fracture fragments are absolute indications for surgery, however a novel closed reduction technique has found success extricating these fragments without the need for surgery. This may be useful in the rural setting or for patients who are unable to undergo surgery for various medical or socioeconomic reasons. The method is described in this paper. It is advised to exercise caution using this novel technique and consult orthopedic surgery if possible, as manipulation of the fracture fragment can potentially harm joint surfaces [1].
References
[1] Boden S, Boden S, Olgun ZD. Novel Technique for Closed Reduction of Incarcerated Medial Epicondyle from the Elbow Joint. Journal of the Pediatric Orthopaedic Society of North America. 2022;4(1):1-6. doi:10.55275/jposna-2022-0012.
[2] Dodds SD, Flanagin BA, Bohl DD, DeLuca PA, Smith BG. Incarcerated medial epicondyle fracture following pediatric elbow dislocation: 11 cases. The Journal of Hand Surgery. 2014;39(9):1739-1745. doi:10.1016/j.jhsa.2014.06.012.
[3] Lewallen L, Elliott M, McIntosh AL, Ho CA. Pediatric elbow dislocations and associated fractures. Children (Basel). 2023;10(6):993. doi:10.3390/children10060993.
[4] Murphy RF, Vuillermin C, Naqvi M, Miller PE, Bae DS, Shore BJ. Early Outcomes of Pediatric Elbow Dislocation—Risk factors associated with morbidity. Journal of Pediatric Orthopaedics. 2017;37(7):440-446. doi:10.1097/bpo.0000000000000676.
[5] Vuillermin C, Donohue K, Miller P, Bauer A, Kramer D, Yen Y. Incarcerated Medial Epicondyle Fractures With Elbow Dislocation: Risk Factors Associated With Morbidity. Journal of Pediatric Orthopaedics. 2019; 39 (9): e647-e651. doi: 10.1097/BPO.0000000000000991.4
[6] Weerakkody Y, Gaillard F. Elbow ossification. Radiopaedia.org. May 2008. doi:10.53347/rid-1263.


